Introduction: since the introduction of tyrosine kinase inhibitors (TKIs), the survival of chronic myeloid leukemia (CML) patients has sharply increased. Three generation of TKIs with different toxicity profiles, including glyco-metabolic alterations (i.e. diabetes mellitus [DM] and impaired fasting glucose [IFG]), are currently available in clinical practice. The risk of developing type 2 diabetes (T2D) reflects the joint effect of genetic predisposition and relevant environmental exposure; genome-wide association studies (GWAS) have identified more than sixty single nucleotide polymorphisms (SNPs) associated with this risk.
Aim: to explore the impact of different TKIs on the development of T2D, especially in relation to the presence of those SNPs showed to have a major involvement in T2D insurgence.
Methods: the study includes 25 consecutive patients affected by CML, who have been treated in first line with continuous TKI therapy (imatinib, dasatinib, or nilotinib) for at least 6 months (mean 54 months, range 8-86). Anthropometric and glyco-metabolic parameters were collected at start of therapy and during last follow-up visit or at switch of therapy. Moreover, we genotyped 17 SNPs in which one of the two alleles has been associated with greater susceptibility to T2D (rs10490072, BCL11A; rs10811661, CDKN2A/2B; rs10923931, NOTCH2; rs1111875, HHEX; rs1801282, PPARG; rs4402960, IGFBP2, rs4607103, ADAMTS9; rs5219, KCNJ11; rs7578597, THADA; rs7903146, TCF7L2; rs7961581, TSPAN8/LGR5; rs864745, JAZF1, rs9472138, VEFGA; rs9939609, FTO; rs1153188, DCD; rs12779790, CDC123/CAMK1D; rs7754840, CDKAL). The Wilcoxon singed-rank test was used to determine the impact of each TKI on glyco-metabolic parameters, whereas the comparison among imatinib, dasatinib, and nilotinib was studied through the Kruskal-Wallis test with post-hoc pairwise comparisons. The latter was also used to analyze the impact of risk alleles of each SNPs on clinical parameters. Statistical analyses were conducted using IBM SPSS Statistics for Macintosh, Version 26.0. Armonk, NY: IBM Corp.
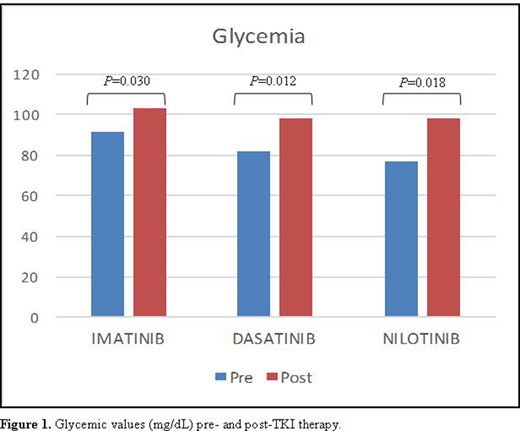
Results: among our study population, 13 (52%) patients were males and the median age at CML diagnosis was 57 years (range, 33-86). Nine (36%) were taking imatinib, 8 (32%) dasatinib, and 8 (32%) nilotinib. Our analysis showed that all TKIs significantly increased glycemic levels (Figure 1), however without reaching the criteria for T2D onset. Furthermore, when analyzing SNPs associated with greater T2D susceptibility (Lyssenko V et al. N Engl J Med 2008), most of the patients (22/25, 88%) had been found to bear more than 12 risk alleles (median 16, range 11-20), so being at higher risk of T2D insurgence. Nevertheless, the effect of the analyzed TKIs on T2D development was not worsened by the presence of these risk alleles. Besides, nilotinib interestingly demonstrated an effect on total cholesterol and LDL level increase (p=0.012 and p=0.017, respectively).
Conclusions: despite the limited size of the cohort, our data suggest that imatinib, dasatinib, and nilotinib similarly does not influence the emergence of T2D, neither when considering the several SNPs known to be clinically related to this comorbidity. Besides, a significant correlation between TKIs administration and glycemic level increase has emerged together with nilotinib influence on other metabolic parameters (i.e. total cholesterol and LDL), confirming similar results of previous studies. Therefore, in clinical practice, glycemic state should not preclude the use of any TKIs, but close monitoring of glyco-metabolic alterations is fundamental to promptly identify any glycemic or lipidic alteration. Updated data with new analyses will be presented later.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal